For at least nine years our health Insurance providers have been saving money by incentivizing unqualified doctors to deny treatment mandated by doctors who do not practice addiction and mental health medicine. And apparently, no one cares.
These denials happen on a regular and on-going basis not only in California, but from coast to coast, and have been public knowledge since at least August 2, 2014, when United States Court of Appeals, Ninth Circuit (CA) found UBH guilty of violating its responsibility to an insured by relying on the false denial written for UBH by Dr. Barbara Center, medical director of Wisconsin-based Prest & Associates. Even though this court case happened in California, Dr. Center still does peer-to-peer reviews not only nationally but in California. Her denial rate is 96%.
Just four months later the CBS News Magazine “Sixty Minutes” broadcast “Denied,” an exposé calling out Anthem for paying doctors like Tim Jack $25,000/month to deny 92% of the cases sent him. I remember him from the days when I was co-founder and CEO of Malibu Beach Recovery Center. He denied residential treatment to an alcoholic took a gun from his father’s drawer and shot up their upscale West Los Angeles neighborhood. When bath salt addicts were reportedly cannibalizing the homeless, he authorized outpatient care only.
We thought this practice would finally end in California when SB 855 (Wiener) became law on January 1, 2021, giving us the most sweeping addiction and mental health parity law in the US, which included a mandate for insurance companies doing peer-to-peer reviews to determine length of care and level of care by using (1) the criteria of the American Society of Addiction Medicine for substance abuse, or (2) in the case of mental health (2) LOCUS.
To our surprise, despite SB 855’s mandate to use ASAM criteria, the denials by the same unqualified doctors continued apace. It meant that up and down California, insurance companies were sending SUD patients home well ahead of the days mandated by ASAM criteria, to relapse and possibly die, become homeless or wards of the State.
All the insurance companies ignored ASAM’s own recommendation that states ensure “plan reviewers and consultants (who are) tasked with reviewing requests for authorization for SUD treatment have the licensure, expertise and training necessary to determine whether the patient meets The ASAM Criteria for the level of care requested by the provider.” Specifically, ASAM recommends that UR determinations concerning service type, service intensity, level of care determination, continued stay, or transfer are made “by or in consultation with a board-certified addiction specialist physician.”
Together with State Senator Dave Cortese, who represents most of Santa Clara County, Summit Estate Recovery Center and others brought SB 999 to make it illegal for the insurance companies to use unqualified doctors to deny treatment determined as needed by ASAM criteria. He wrote:
“SB 999 will save lives. California law requires that insurance companies cover treatment for addiction recovery, yet many are still denied the critical services they need to survive…We must remove the financial incentives that exist for health plans to deny patients’ life-saving treatment.”
SB 999 also called for normal working conditions for peer-to-peer reviews - no more 5 a.m. PST calls about reviews that need to begin in 30 minutes. No reviews refused because the treating California doctor calls the insurance company doctor who also lives in California at 4 p.m. and is told that 4 p.m. is “after close of business.” No more denials cut and pasted from other denials (without changing the pronoun of the patient). No more doctors who refuse to reveal their full names, their addiction credentials (if any) or the states where they were licensed.
In November 2021 Summit and several billing companies began keeping score. The results of peer-to-peer reviews for 38 facilities were monthly reported. The Scoreboard, now 19 months old, shows clearly that most active Prest & Associates “external” doctors have denial rates ranging from 75%-100%. The main Anthem “internal” doctors who uphold the Prest denials themselves have denial rates ranging from 79%-100%. MSN doctors deny 82%-88% of the time. There are other doctors with lower denial rates, but they are assigned very few peer-to-peer reviews.
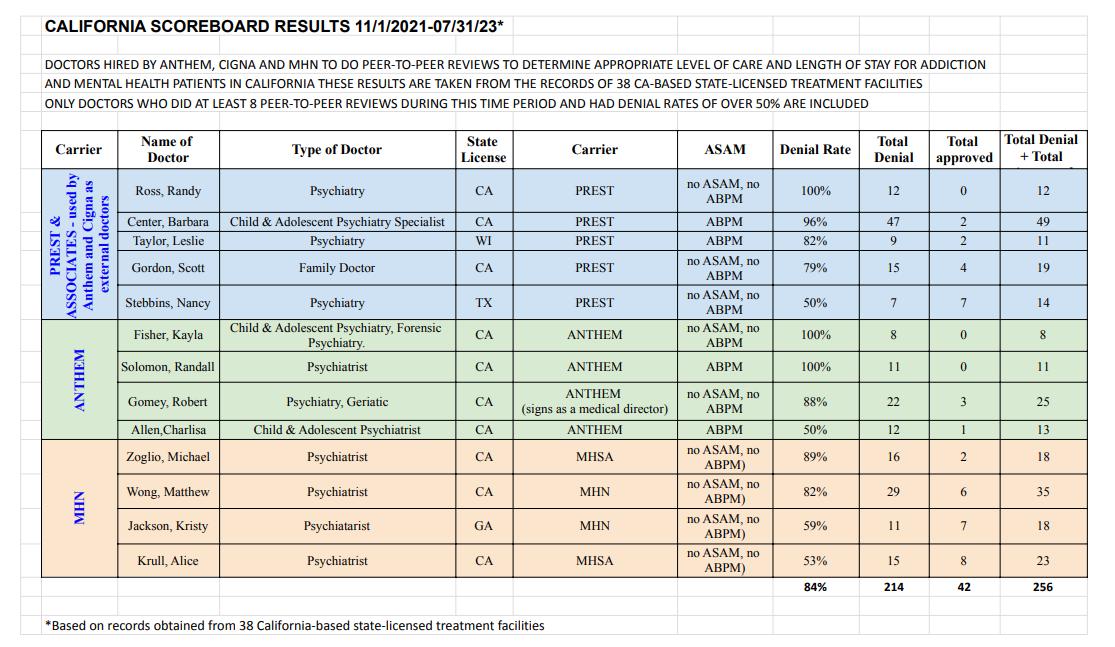
Not one of the almost 80 external and internal doctors hired by insurance companies (mostly Anthem) to do peer-to-peer reviews for addiction patients since November 1, 2021, is ASAM or CSAM accredited, or make their decisions based on ASAM criteria although they frequently admit to knowing ASAM criteria.
It has long been established in the addiction industry that the Gold Standard for residential treatment is plus or minus 28 days. The doctors who incentivize to deny often cut treatment off as early as 10 days.
The insurance lobby objected strenuously to SB 999. Three DMHC lawyers who supported the Lobby met with us personally to explain that SB 999 would “create an arduous new process which would substantially limit who is allowed to conduct utilization reviews.” Fact: There are 6,000 ASAM credentialed doctors in the United States.
Our then lobbyist had to remind them during our meeting, also attended by a representative of Senator Cortese, they were reading word for word from an insurance lobby SB 999 opposition document.
After hearing testimony from clinicians and victims, members of the State Senate and Assembly Health and Appropriations Committees understood the damage being done to substance abuse and mental health patients by the insurance companies and passed SB 999. SB 999 then passed votes of both houses.
When the bill landed on Governor Newsom’s desk, to our great surprise, it was vetoed. The Governor said our bill was premature because 21 months after SB 855 became law, the regulations for implementing it still had not yet been finalized by the Department of Insurance (DOI) and the Department of Managed Health Care (DMHC). He wrote that he shared Senator Cortese’s goal of ensuring patients can receive the behavioral health care they need when they need it…and assured Senator Cortese that the regulations would address the issues ‘by requiring the use of unbiased mental health and substance use disorder clinical standards in coverage reviews and mandating the appropriate training and oversight of staff performing those reviews.”
While waiting for the two agencies to act, at the suggestion of the Kennedy Forum, Summit began to request Independent Medical Reviews (IMR) through the DOI and DMHC to overturn the illegal decisions, all of which we won. Summit was not the only facility to win IMRs. In December 2022 Bloomberg News reported that 66% of all IMRs related to addiction and mental health, filed after SB 855 became law, overturned the illegal decisions.
This would seem to be good news, but it must be noted that in most cases, when an insurance company denies treatment mandated by ASAM, the patients are either discharged to a lower level of care or sent home. Not every patient can privately pay for the denied days, and not every treatment center can afford to scholarship the denied days of mandated treatment. In all but the most extreme cases, the IMRs are won months after the unqualified doctors have denied treatment.
After a hearing in December 2022, the DOI which regulates about 20% of California’s health insurance plans, agreed to include a regulation requiring only qualified doctors practicing addiction medicine or mental health medicine to do peer-to-peer reviews.
We expected the DMHC, which regulates the other 80% of the health plans, to follow suit. Unfortunately, their final draft regs published June 19, 2023, do nothing to stop insurance companies from incentivizing unqualified doctors to deny when doing peer-to-peer reviews.
Meanwhile, as this is a national problem, we are enroute to Washington, DC to drum up support for strict guidelines for health insurance policies governed by ERISA. I urge all interested treatment center owners and billers to help by (1) contributing information to our Scoreboard each month, (2) filing Independent Medical Reviews (I will teach you how) and (3) contacting your state congressional representatives about this outrageous behavior that health insurance companies have been using to pad their bank accounts for at least a decade. Ask them to open investigations into Prest & Associates and the insurance company doctors who deny needed health care.
Feel free to write to me at joan@summitestate.com.
Joan Borsten is the co-founder and former CEO of Malibu Beach Recovery Center, co-founder and former Vice President of the Addiction Treatment Advocacy Coalition and currently Executive Director of Summit Estate Recovery Center, located in Silicon Valley.


