Clearly Defining Relapse Is Crucial
If you ask someone in the medical field about relapse, they most likely will say relapse is going back to an active state of a disease after a period of remission. When you ask someone recovering from inappropriate use of medications, including using alcohol or other drugs they may say it’s going back to using the substance again.
While that definition is partially correct, it can be dangerous, especially if people thinks the only criteria for recovery is abstinence. Another common definition of relapse is that a person goes back to their addiction process. The full explanation of relapse is much more complex and must include not only maintaining abstinence or an appropriate medication management plan but also stop following their mental health treatment plan or sabotaging their chronic pain management plan.
- People can head back towards relapse without even thinking of using
- They can start sabotaging their effective chronic pain management plan
- People also stop following their mental health treatment plan
What many people don’t realize is that the chemical use or coming out of remission is not the beginning of a relapse. It is the final step in an ongoing relapse process. In addition, relapse is a common symptom of a medication use disorder or other chemical use disorders, and one-third to two-thirds of all recovering people in chemical recovery relapse despite their best intentions not to do so. The good news is we can take the mystery out of relapse and increase people’s chances for positive recovery without a chemical relapse episode.
If someone is also living with a coexisting disorder—e.g., chronic pain, depression, PTSD or an anxiety disorder—the instance of relapse can be even higher because these other problems can easily become relapse justifications. Fortunately, the risk of relapse can be lowered if recovering people are exposed to education and training about relapse prevention and how to deal more effectively with all of their coexisting problems. Prevention is much easier than crisis management.
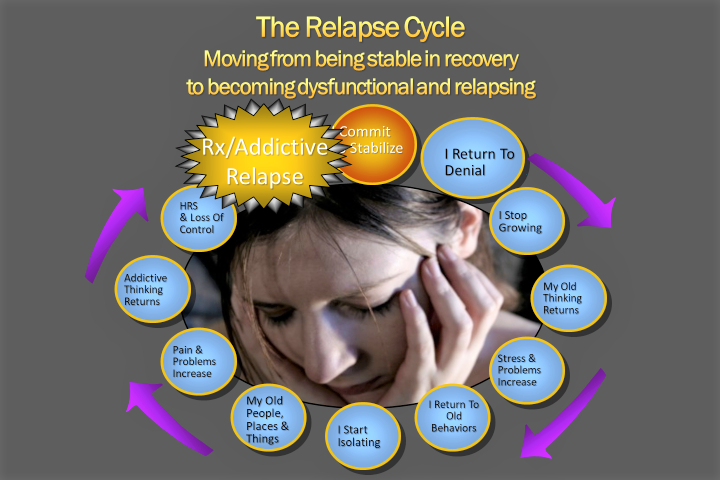
I believe relapse education must start with a new definition of relapse. The definition I propose and share with my patients is: Relapse is the process of becoming dysfunctional in your recovery process. Relapse is a progressive series of events that takes people from a stable recovery through various stages of dysfunction, and eventually go back to using inappropriate medications, alcohol or their other drugs of abuse.
Relapse is the process of becoming dysfunctional in your recovery!
I tell my patients that when you start on the slide to relapse you will undergo many changes. One of the first changes is a return to denial that at first has nothing to do with substance use, sabotaging your pain management plan or addictive behaviors. In other words, you begin denying that you need to work a program of responsible living, healthy communication with others, and constantly looking at yourself for evidence of progress and problems in yourself and your life. To deny these needs leads to thinking problems.
Now instead of responsible recovery-prone positive thinking people start experiencing relapse-prone negative thinking and eventually euphoric recall. This negative thinking leads to experiencing uncomfortable and/or painful emotions. These feelings produce self-defeating urges which are often followed by self-destructive behaviors or ineffective chronic pain management. Inappropriate use of medications, alcohol or other drugs may not be an option in the early stages of relapse, but the negative behaviors often set people up to experience even more problems including increased pain flare ups.
Being in recovery demands developing a new set of tools. People need to learn how to move from a problem-centered lifestyle to a recovery-centered one. In the same way, when they are trying to remain in recovery, they need to learn all that they can about the sobriety-based symptoms of a substance use disorder (medications, alcohol or other drugs) and to develop new tools for coping with these symptoms.
Another important task for relapse prone people is to be able to identify and manage their patterns of self-defeating thoughts and behaviors that are called relapse warning signs and high-risk situations.
Recovery Prone and Relapse Prone Ways Of Managing Stuck Points
When educating my patients about relapse prevention I let them know it is normal and natural to hit stuck points on their recovery journey. These stuck points are what Terence T. Gorski calls Warning Signs and High-Risk Situations. The difference between and warning sign and high-risk situation is that high risk situations include thinking about using substance or have urges or cravings to use inappropriate medication including alcohol or other drugs.
Recovery-Prone People
When people are in a recovery prone mode, they are working a proactive recovery program in all areas of their lives – Biological, Psychological, Social and Spiritual. When they hit a stuck point, they recognize it’s a warning sign that needs attention. They also accept that it is normal to hit stuck points in their recovery. They can decide to effectively manage their suck point. They are able to ask for help and respond with authentic action without procrastination. In his book Passages Through Recovery, Terence T. Gorski calls this RADAR.
- Recognize
- Accept
- Decide
- Ask for Help
- Respond with Action
Relapse-Prone People
People who are not working a good program can hit stuck points with a self-defeating style of coping. Their first step is to evade or deny that they are having a problem. Then since the problem is still there and possibly worsening, they start experiencing increased levels of stress. They start using old self-defeating compulsive or impulsive patterns. The isolate and avoid anyone who might recognize they are having a problem. Their problems worsen and they start evading and denying these new problems. And then the cycle keeps spiraling downward. In Passages Through Recovery Mr. Gorski calls this ESCAPE.
- Evade/Deny the Problems
- Stress Increases
- Compulsive/Impulsive Behaviors to Cope
- Avoidance and Isolation Tendencies
- Problems Worsen
- Evade/Deny the New problems
Relapse Prevention Planning Is Crucial
As I mentioned earlier, the term “Relapse Prevention” is so misunderstood in all types of healthcare treatment. Medically we know of many diseases like Cancer, Diabetes, Heart Disease, Hypertension etc. that all have high incidents of “relapse” after a period of remission. This means that through treatment they reach a stable place and for whatever reason days, weeks, months or sometimes years later, they “relapse” or go back into the active phase of their medical condition. Relapse prevention needs to take all this into account.
In Substance Abuse (or Addiction) treatment programs they also see a high rate of relapse. However, many people do not really relapse because they were never in remission (or Recovery) in the first place.
My Criteria For Assessing Early Recovery
- The person has an accurate and objective understanding of a substance use disorder
- They are able to admit they meet the criteria for a substance use disorder
- They are able to manage the shame, guilt and remorse that comes with this diagnosis
- They have hope and belief that recovery is possible and preferable to the old ways
- They are willing and able to execute the Bio-Psycho-Social-Spiritual footwork recovery requires
- They have a 60-90-day period of abstinence and/or they are following an appropriate medication management agreement
In mental health treatment people stopping one or more of their treatment plan components often leads to a worsening of their mental health problem. In chronic pain management relapse episodes are often called pain flare ups. Meaning that the patient has been on a treatment protocol that kept their pain at acceptable levels. Then for some reason – sometimes identifiable and sometimes not – they start experiencing a pain flare up sometimes way above their acceptable levels of pain.
With mental health issues like PTSD, Depression, Anxiety etc. there are also periods where the condition is in remission or stable and then the patients’ conditions worsen. This also often happens because of identifiable and treatable reasons.
Relapse Prevention is Crucial for the Whole Person
I tell my patients that as they embark on their new more effective chronic pain management journey, it is important to continue learning even more non-pharmacological, holistic pain management tools. Then they need to develop an initial relapse prevention plan that will help them identify their high-risk situations that include ineffective pain management or self-sabotage as well as triggers for other coexisting disorders.
It is crucial to have a relapse prevention plan in place that addresses both the high-risk pain situations as well as any core substance use disorders or other coexisting psychological issues such as depression, anxiety, PTSD etc. At this point I tell my patients that they are beginning an exciting, and possibly frightening, journey of self-discovery. At this point it’s hold on tight and hang in there because the journey is worth it. It’s onward and upward with hope and gratitude.